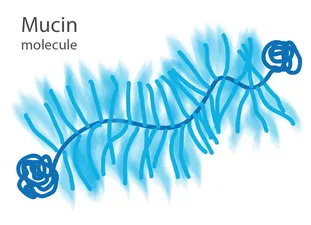
In the past years, we and others have pinpointed different application areas, where purified mucins can be valuable components of materials or devices. In the following, we give a brief overview over selected application fields that could benefit from mucins.
Contact Lenses
With a prevalence of more than 10 %, keratoconjunctivitis sicca (commonly known as dry eye syndrome) is one of the most frequent forms of ocular diseases; among contact lens wearers, this condition occurs even more often. Mucins are a key component of the ocular tear film and also here serve as a molecular lubricant. In the absence of a proper mucinous lubrication layer on the cornea surface, increased friction and tissue damage induced by contact lens sliding leads to discomfort. We have recently shown that purified gastric mucins efficiently prevent damage on the cornea. This protective effect can be achieved in two different ways: mucin solutions can be used as ‘artificial tears’ (eye drops) for cornea lubrication or as a molecular coating on contact lenses. Importantly, such mucin coatings help maintaining the excellent transparency of contact lenses by reducing the adsorption of lipids from the tear film.
Literature:
Rickert et al., Highly Transparent Covalent Mucin Coatings Improve the Wettability and Tribology of Hydrophobic Contact Lenses. ACS Applied Materials & Interfaces (2020)
Winkeljann et al., Mucin Coatings Prevent Tissue Damage at the Cornea–Contact Lens Interface, Advanced Materials Interfaces (2017)
Hofmann et al., In-vitro method for determining corneal tissue friction and damage due to contact lens sliding, Biotribology (2016)
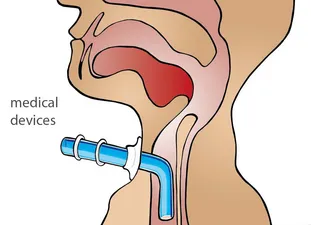
Medical Devices
As a part of surgery or post-surgery measures, catheters, ventilation tubes or stents are inserted into the human body. Those tubes are typically made from polymers and cause friction on the tissue epithelia they rub across, which causes discomfort and may damage the tissue. Moreover, if those artificial objects remain in the body for extended time periods (several days up to weeks), another issue starts to play a role: biofouling, i.e., the uncontrolled deposition of proteins or other biomolecules onto the surface of the tubes which is typically followed by colonization of bacteria. This process negatively impacts the proper function of the tubes and can also lead to inflammation. Under lab conditions, mucin-coatings of synthetic materials such as polystyrene and glass were already generated by passive adsorption and could successfully reduce biofouling events. Generating stable, covalent mucin coatings on medical devices such as catheters or ventilation tubes could greatly improve their biocompatibility.
Literature:
Winkeljann et al., Covalent mucin coatings form stable anti-biofouling layers on a broad range of medical polymer materials. Advanced Materials Interfaces (2020)
Song et al., Bioinspired Dopamine/Mucin Coatings Provide Lubricity, Wear Protection and Cell Repellent Properties for Medical Applications. Advanced Healthcare Materials (2020)
Janeiro et al., Mucin Covalently Bonded to Microfibers Improves the Patency of Vascular Grafts, Tissue Engineering Part A (2014)
Wound Treatment
Bacterial and viral infections still represent a major cause of diseases that may lead to severe illness or even death. In healthy adults, the intact skin provides a first barrier against such microbial infections. However, in situations where this natural barrier is compromised, e.g. trauma, injuries, or surgery, the risk of contracting an infectious disease is drastically increased. In contrast to the outer skin, all wet epithelia are covered with mucus, where the mucus serves as an initial barrier against microbial attack. Indeed, mucins combine anti-bacterial and anti-viral properties. Thus, mucin based wound gels could be a promising tool to overcome the temporal inability of the damaged skin to protect the underlying tissue from infections. By combining mucins with other biopolymers, e.g., methylcellulose or hyaluronic acid, we can create functional materials in the form of gels or films. Here, the mechanical properties of the mucin-based materials can be adjusted to form a stable cover. Such mucin-based materials can be enriched with drugs that are then released in a controlled manner.
Literature:
Kimna et al., Multifunctional ‘Janus-type’ bilayer films combine broad-range tissue adhesion with guided drug release. Advanced Functional Materials (2022)
Nowald et al., A Selective Mucin/Methylcellulose Hybrid Gel with Tailored Mechanical Properties, Macromolecular Bioscience (2016)
Duffy et al., Covalently-crosslinked mucin biopolymer hydrogels for sustained drug delivery, Acta Biomaterialia (2015)
Lieleg et al., Mucin biopolymers as broad-spectrum antiviral agents, Biomacromolecules (2012)
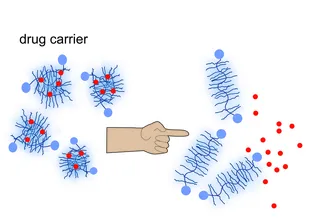
Drug Carriers
Many pharmaceuticals require some sort of packaging so they can be successfully delivered to their target location in the human body. Encapsulating pharmaceuticals into nanoparticles is a very useful strategy for this purpose, and using mucins for the has recently turned out to be an excellent option. By making use of DNA-nanotechnology, we can build mucin-based nanocarriers such that only selected target cells are able to open those carriers. However, also mucin coatings have the ability to carry drug molecules and to liberate them on demand, e.g., when the coating comes into contact with body fluids or when it is exposed to fever-like temperatures. With the latter strategy, implants could be provided with a layer holding antibiotics that are only released when required.
Literature:
Kimna et al., DNA Strands Trigger the Intracellular Release of Drugs from Mucin-Based Nanocarriers. ACS Nano (2020)
Kimna et al., Smart biopolymer-based multi-layers enable consecutive drug release events on demand. Advanced Materials Interfaces (2020)
Duffy et al., Covalently-crosslinked mucin biopolymer hydrogels for sustained drug delivery. Acta Biomaterialia (2015)
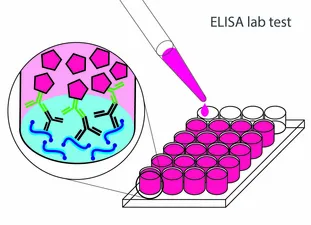
ELISA Lab Test
For the biochemical analysis of biological mucus samples, e.g., as part of a clinical evaluation of mucus specimens from patients with cystic fibrosis, different lab tests are available. One of the most frequent lab tests used to identify certain biomolecules is ELISA (Enzyme-linked Immunosorbent Assay), which makes use of a set of two antibodies to detect target molecules and to visualize them with a chromophore reaction. However, to give quantitative results, this well-established assay requires purified solutions of the target molecule as a standard. Currently, the compromised structure of industrially purified gastric mucins prevents their detection by antibodies – although the very same antibodies do detect those gastric mucins if they are manually purified in the lab. Thus, a better availability of highly functional purified mucins will simplify the analysis of clinical mucus samples and thus could contribute to a better detection of mucus-related diseases and their treatment.
Mouth Spray
Especially among the elderly population, but also as a side-effect of chemotherapy treatment, many people suffer from a dry mouthfeel (xerostomia). Xerostomia not only leads to a permanent feeling of oral discomfort but also makes the ingestion of food difficult: without a proper oral lubricant, chewing and swallowing becomes complicated and very unpleasant. The missing lubricity in the oral cavity of dry mouth patients is mostly due to a reduced or altered production of salivary mucins. Thus, using mucin containing aqueous solutions for the treatment of xerostomia symptoms can be a good option – especially since mucin-based solutions were shown to possess a similar lubricating potential as human saliva. Moreover, such mucin solutions are still very good lubricants when they are diluted (as it can occur after drinking fluids) are when they get in contact with salt (e.g., during eating).
Literature:
Song et al., The lubricity of mucin solutions is robust towards changes in physiological conditions. ACS Applied Bio Materials (2019)
Winkeljann et al., Oscillatory Tribology Performed with a Commercial Shear Rheometer, Biotribology (2018)
Biegler et al., Cationic astringents alter the tribological and rheological properties of human saliva and salivary mucin solutions, Biotribology (2016)